The gallbladder is our odd organ, located under the liver behind the ribs on the right side. The greenish-brownish bile produced by the liver helps digest fats. This fluid is stored in the gallbladder, where it thickens before passing through the bile ducts into the small intestine. The gallbladder is not an essential organ, so there are no negative consequences of removing it.
The most common disease of the gallbladder is the presence of gallstones, which block the flow of bile from the gallbladder, causing swelling and inflammation, which can lead to further severe abdominal pain and indigestion.
They can range in size from 1 mm to several cm. Obesity, diabetes, metabolic disorders, liver diseases may predispose to their development.
In the case of gallstones, surgery is the safest way to treat them and prevent further complications such as jaundice or pancreatitis.
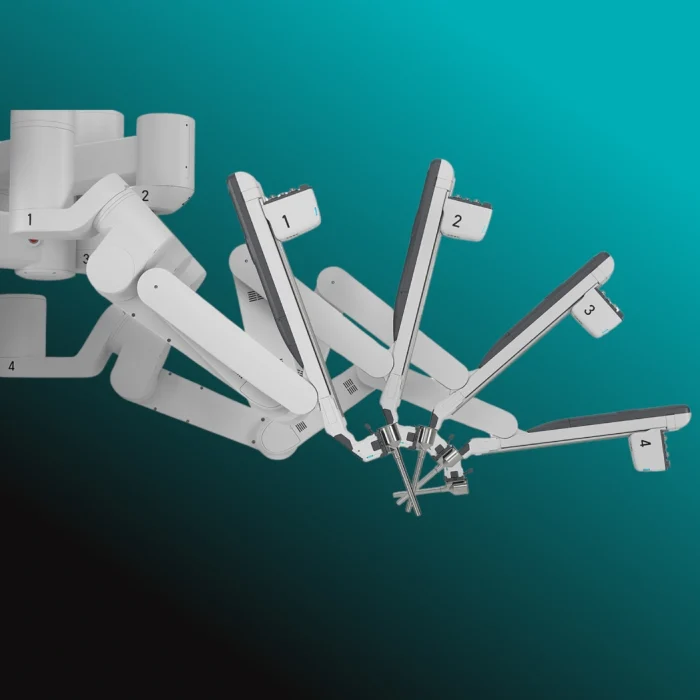
In addition to the laparoscopic procedure, gallbladder removal is also performed using the da Vinci robot assisted method. This is only available in private healthcare in our country at the Wáberer Medical Center.
Laparoscopic surgery is a branch of endoscopy in which surgery is performed in the abdominal cavity. The laparoscope has a thin tube with a camera at the end, so that an image can be followed through an optical device inside the body. The laparoscope and surgical instruments are inserted through several small incisions (0.5-1.5 cm) to carry out each step of the operation.
Advantages of the procedure:
– less post-operative pain
– shorter hospital stay
– shorter recovery time
– less visible, smaller scars, faster wound healing
Less time to repair, shorter incision, shorter healing time, shorter healing time:
– open surgery (mainly in acute cases, with a larger incision)
– treatment of gallstones with medication (can be reduced, dissolved)
Gallbladder inflammation can in some cases be treated conservatively with prolonged antibiotic therapy, along with analgesics and antispasmodics.
If the inflammation worsens, surgery becomes a worse option in a worse setting, but becomes urgent. If conservative therapy is effective, removal of the gallbladder is still recommended 6 weeks after the spasmodic period. Your doctor will explain the details if this is an option for you.
The operation is needed because of inflammation of the gallbladder wall, most often caused by a stone in the gallbladder. The procedure is best performed within 48-72 hours of the onset of inflammation. Inflammation can cause the gallbladder wall to become permeable, which can lead to peritonitis and liver abscess. Typically, gallbladder inflammation causes pain below the right costal arch radiating to the scapulae, and may also cause fever and temperature. Prolonged gallbladder inflammation can cause bloodstream infection with potentially fatal outcomes.
You will most likely arrive on the day of your operation, but rarely do we ask someone to book your room the night before. Nevertheless, we will carry out the necessary tests 1-2 weeks before the planned day of surgery, which may include laboratory tests, ECG, X-ray and anaesthesia if necessary.
If you smoke, try to quit at least 2 weeks before surgery to reduce the known adverse effects on wound infection and lung function. If necessary, seek help. However, it is important that you do not smoke for 24 hours before the operation.
The operation is performed under general anaesthesia. You can read more about what the anaesthetist does to ensure your safety and comfort and how you can prepare for the operation in the anaesthetic leaflet.
Through a small incision made above the navel, the abdominal cavity is inflated with carbon dioxide gas through a special device. The laparoscope is a thin tube with a camera at the end, which is used to navigate inside the abdomen, to view the abdomen, and to follow the surgery through a large screen. We make 3-4 small incisions in the upper abdomen to insert the thin long instruments, the small artery supplying the gallbladder and the gallbladder duct are dissected, closed with plastic clips and then cut. The gall bladder is dissected from its bed and removed through a small incision, together with the stones, and sent for histological examination. A silicone tube (drain) is left in the abdominal cavity. The surgical wounds are then closed. The surgery takes on average 30-60 minutes, which is extended by approximately 30-40 minutes with the preparation, anaesthesia and closing steps.
– improves well-being
– digestive problems may disappear
– severe abdominal pains improve
There are risks involved in having the operation, and your doctor will explain these before you give consent. Please ask any questions you may have.
As with any laparoscopic surgery, it may be necessary to convert to open surgery (conversion) during a gall bladder removal. Internal scarring due to gall bladder inflammation, anatomical abnormalities, anatomical variations may require conversion to open surgery during surgery.
Possible complications of laparoscopic gall bladder removal:
Bile duct injury may require extension of the operation, drainage of the bile ducts during surgery. In the case of post-operative bile leakage, horseshoe aspiration may be used to detect the cause of the leakage and then to eliminate it by splinting the bile ducts (stenting). If this procedure is not successful, another operation may be performed.
The operation may involve intestinal or vascular damage, some of which can be treated with a laparoscope, others with open surgery.
Stones in the bile ducts can lead to bile duct stones and pancreatitis, which may require endoscopic surgery.
– The skin of the abdomen around the scar may become numb, but this usually resolves itself within 2-3 months
Deep vein thrombosis (clot formation in the large veins of the lower limb or pelvis) and consequent pulmonary embolism may develop, for which we recommend wearing elastic stockings and administering low molecular weight heparin after surgery.
During the operation, you will sleep and feel no pain. Upon waking, you can expect to experience some discomfort, and we will do our best to minimise this, or if it has developed, to alleviate it.
Due to the nature of the surgical technique, there may be some soreness in one or possibly both shoulders, which may be caused by the tensioning of the diaphragm during the operation (inflation of the abdomen with carbon dioxide).
There may also be some discomfort around incisions, which should also improve considerably with the use of painkillers. It’s important to take painkillers regularly for the first few days, not just when you’re in a lot of pain, so that they have a more even effect. Painkillers will gradually become unnecessary over time. Please contact us if you are not getting enough pain relief. It is also important that you do not exceed the maximum daily dose indicated in the prescription.
The effects of sleeping pills will wear off completely in 24-48 hours, but it is not necessary – or even good – to stay in bed during this time. Most people can return to work within 1-2 weeks.
Please avoid the immediate post-operative period: